 Information for Patients following Heart Attack
Information for Patients following Heart Attack -
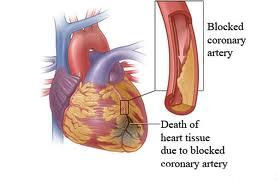
WHAT IS A HEART ATTACK?
Heart attack or myocardial infarct (MI) is the result of a blockage in the arteries that supply oxygen-containing blood to the heart muscle (coronary arteries). This blockage is usually a blood clot. This lack of blood flow means that part of the heart muscle is starved of oxygen for a period of time and may become permanently damaged.
The symptoms associated with a heart attack can be variable, ranging from severe central chest pain to mild chest discomfort or feeling generally unwell. The length of time that the pain may last and the distribution of pain in the body might also be different from one person to another. In some cases the pain has been mistaken for indigestion.
WHAT CAUSES A HEART ATTACK?
Heart attacks are usually the result of a process that has been going on for some time resulting in damage to the coronary arteries – Coronary Heart Disease. The arteries over time become narrowed as a result of a build-up of fatty deposits in the walls of the arteries (atherosclerosis). This narrowing can mean that the arteries are not able to supply enough oxygen rich blood to the heart muscle at times when it requires more than usual, for example during exercise.
RISK FACTORS
The following are a list of things that increase the risk of having coronary heart disease:
- Physical Inactivity
- High Blood Pressure
- Smoking
- High Blood Cholesterol
- Being overweight
- Diabetes
- Family History of Heart Disease
-
WHAT HAPPENS TO THE HEART AFTER THE HEART ATTACK?
The recovery process begins in the first couple of days. The damaged heart muscle is replaced with scar tissue. In most cases the scar itself is strong enough for the heart to pump just as well as normal. However, a heart attack at times can cause more severe damage to the heart tissue and the pumping action of the heart is affected. This may result in breathlessness, tiredness and swollen ankles. This condition is called Heart Failure.
REMEMBER:
- There is much less risk of another heart attack as you recover
- Your heart is one the toughest muscles in the body and it recovers very quickly
- Physical work and activity will not cause another heart attack
- It is normal to feel tired, but this will pass. There will be good days and bad days
- Most of the risk factors associated with heart attacks you can change yourself, and it is never too late!
- Most people make a full recovery from a heart attack returning to a normal life
- Once fully recovered many people actually feel better than they did before their heart attack
-
WHAT SHOULD I DO WHILST IN HOSPITAL?
The following programme is a guide of what activity you will be allowed to do whilst an inpatient immediately following a heart attack. Remember, this is a guide only and some patients may achieve full physical activity sooner.
STAGE 1
- Complete bed rest
- Use of beside commode
- Bed bath
- Shave self and clean own teeth
- Active ankle movement- foot circles and pointing toes. Deep breathing for five minutes every hour whilst awake.
STAGE 2
- Self wash with assistance
- Bedside commode/wheel to toilet
- Sit on edge of bed to swing legs for 15 minutes twice daily
- Sit out of bed for ½ to 1 hour twice daily
STAGE 3
- Self wash with assistance if required
- Wheeled to toilet
- Sit out of bed as tolerated
- At least one rest period during the day
STAGE 4
- Sit out of bed as tolerated
- Walk to the toilet
- Walk around the bed at least three times daily
- At least one rest period during the day
STAGE 5
- Walk to the toilet
- Self wash in bathroom
- Walk the length of the ward twice daily
- At least one rest period during the day
STAGE 6
- Shower or bath – supervised
- Walk the length of the ward four times daily
- At least one rest period during the day
STAGE 7
- Shower or bath – unsupervised
- Walk the length of the ward six times daily
- Walk up one flight of stairs supervised
- At lest one rest period during the day
-
GOING HOME AFTER A HEART ATTACK
Most people are happy to be able to go home. However, you may feel worried about leaving the carefully monitored environment of the hospital. If possible try to arrange for someone to stay with you for a couple of weeks.
When you get home you or a relative/partner should inform the Doctor that you have returned from hospital. You will also need to give the Doctor the letter the hospital has given you outlining the treatment you received whilst there and the medications you are to take. Your Doctor will be responsible for providing repeat prescriptions of these medications.
It is quite common to feel depressed when you get home. You don't need to worry too much about this, as it is a natural reaction. If you find that this continues contact your Doctor or talk to the staff at the cardiac rehabilitation programme.
For the first few days take things easy and try to do the same amount of moving around as you did whilst in hospital. The following can be used as a guide:
WEEK ONEAFTER WEEK ONEDO:
- Get up and dressed each day
- Walk around the house
- Walk up/down the stairs at a comfortable pace up to two times daily
- Take a bath or shower
- Shampoo your hair
- Watch TV, play cards, read etc...
- Receive visitors at home (try and limit it to about 4/day)
- Simple household chores – washing dishes, laying the table
- Take at least one rest period during the day
- Aim for 6-10 hours sleep a night
- Do stage one of the walking programme outlined later in this leaflet
DON'T:
- Drive the car for one month
- Play sports or attend sports matches
- Lift, push or drag heavy objects
- Garden
- Vacuum, make the bed, carry loads of washing or hang out clothes on the line
REMEMBER:
- Do not be over cautious. Your heart is already on the mend; do not be frightened of activity
- Partners must be aware of not being too over-protective. In fact, wrapping your partner up in cotton wool may be the worst thing for them. Your task is to help your partner gently return to activity and a normal life
- Follow the outpatient activity guide that is provided later in this leaflet. However, use this as a guide only as everyone progresses at different rates
- Take someone with you when you go out of the house for the first time
- Remember you are alive and getting stronger all the time
-
RETURNING TO EVERYDAY LIFE

Work:
Expect to return to work in 6-8 weeks. It is a good idea to return gradually starting out part-time and gradually increasing the hours. It may help to discuss with your employer, the consultant and the cardiac rehabilitation team what will be the most appropriate for you.
Driving:
You may resume driving after four weeks if you have an ordinary licence. Those with specialised licences may need to undergo further tests to ensure they are fit to drive. Remember that driving is a stressful activity, so try to stay calm!


Sex:
It is understandable to be nervous about resuming sexual activity. Sexual activity increases the heart rate and blood pressure, which increases the amount of work the heart, has to do. In some people this can lead to breathlessness and chest pain. However, if you are able to walk 300 yards or climb two flights of stairs with no chest pain or breathlessness then it is safe to resume sexual activity two to three weeks after the heart attack.
Alcohol:
During the first few weeks after your heart attack it is best to limit the amount of alcohol you drink, and be aware that it may affect any sleeping tablets you are taking. If you are on anti-coagulation tablets such as warfarin it is particularly important not to binge drink as this will impact on how the drug is processed by your system. In the long term you may wish to resume moderate alcohol consumption. Further information regarding this is provided in the diet section of this leaflet.

-
OUTPATIENT WALKING PROGRAMME
If you have any difficulty in achieving either the distance or the time prescribed, you should return to the previous stage for two days and then try again to advance to the next stage.
Preparation for walking:
- Do not attempt to walk when you are feeling tired, when the weather is freezing cold or very windy and within one hour of a bath or shower
- Wear comfortable clothing and footwear
- Walk in daylight
- Walk on level ground (as far as this is possible)
- Wear a watch
- Take your GTN with you
- In cold weather dress up warmly and wear a scarf loosely over your mouth and nose. Do not get up from your chair by the fire and go straight outside. Instead do some warming up exercises before you head out
- After your walk take a rest
- If you experience any of the following symptoms with exercise you should reduce your walking distance for a few days
- Chest pain
- Excessive breathlessness, which persists for more than 10 minutes after exercise
- Dizziness or faintness
- Nausea or vomiting after exercise
- Prolonged tiredness, lasting for more than 24 hours after exercise
- If you always experience chest pain while walking, you may find it helpful to use your GTN before you set out. Repeat as required for further pain. As you become fitter you should require less GTN
-
HOW TO REDUCE YOUR RISK FACTORS
- Eating more fruit and vegetables
- Eating less fat and reducing cholesterol
- Eat more fish and fish oil
- Stay a healthy weight
- Reducing Salt Intake
- Moderate Drinking
- Exercise
- Medication
 Key Focus Areas of STEMI INDIA
Key Focus Areas of STEMI INDIA  |
How to start a Primary PCI program |
 |
Reducing D to B times |
 |
Mastering the procedure and dealing with complications |
 |
Role of thrombolysis in the STEMI era |
 |
Management of arrhythmias in the CCU |
 |
Role of Echocardiography in diagnosis and management of STEMI |
 |
Mechanical complications in STEMI |











